By Prof. Dr. Jaideep Malhotra
Director & IVF Specialist – Rainbow IVF
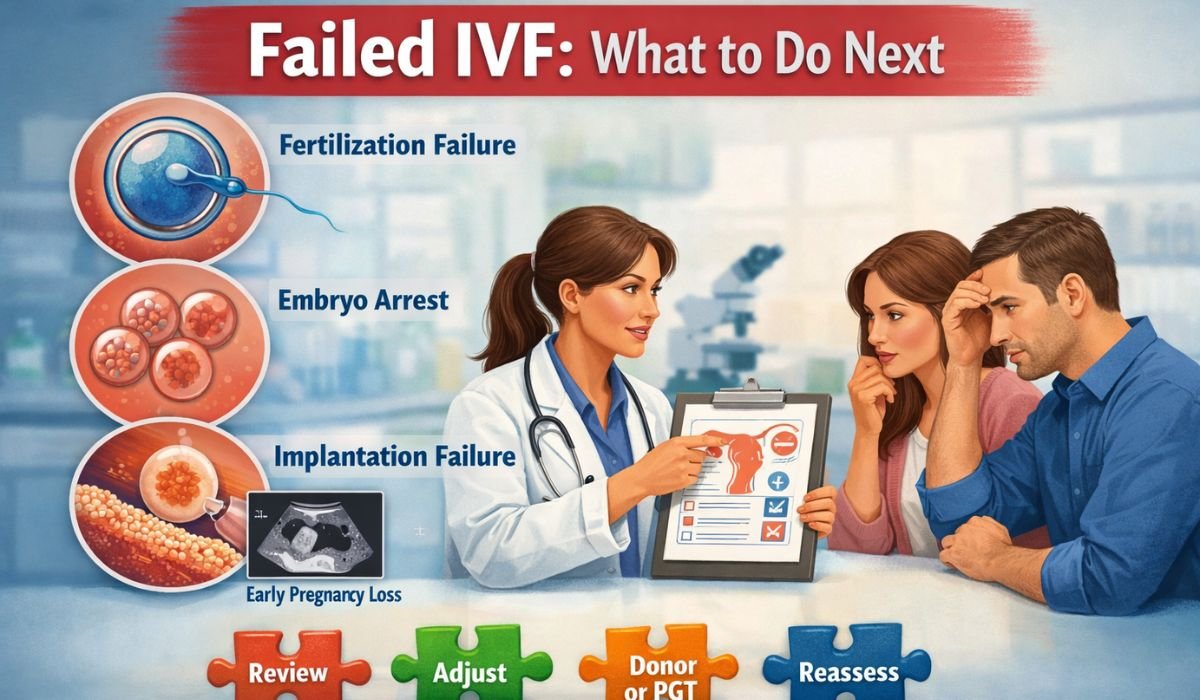
If your IVF cycle has failed once or twice, the most common mistake is rushing into the next cycle without understanding what went wrong.
IVF failure is rarely random. In most cases, something specific was missed, underestimated, or repeated without correction. Repeating the same approach without review often leads to the same result.
Experienced IVF doctors do not simply repeat cycles. They carefully review hormonal preparation, embryo quality, uterine readiness, male factors, and timing before planning the next attempt.
Below is a clear explanation of what doctors medically check before starting the next IVF cycle.
1. Was Hormonal Preparation Truly Optimal?
“Normal” blood reports do not always mean correct preparation.
Doctors reassess:
- FSH, LH, and AMH patterns, not just single values
- Thyroid and prolactin levels at the time of embryo transfer
- Progesterone timing and dosage (one of the most common errors)
Clear fact:
If progesterone is started too early or too late, even a good embryo will fail to implant.
2. Embryo Quality vs Laboratory Quality
Being told “the embryo was good” is not enough.
Doctors review:
- Whether Day-3 or Day-5 embryo transfer was the right decision
- Embryology lab conditions (temperature stability, culture media)
- How embryos were handled during transfer
Hard truth:
The same eggs and sperm can give very different outcomes in different labs.
Lab quality matters as much as embryo quality.
3. Was the Uterus Truly Ready for Implantation?
Endometrial thickness alone does not guarantee success.
Doctors check:
- Endometrial pattern, not just thickness
- Blood flow to the uterus
- Polyps, fibroids, adhesions, or subtle uterine issues
- Whether embryo transfer was technically easy or difficult
Reality:
If the uterus is not receptive, blaming the embryo is incorrect.
4. Was the Male Factor Properly Re-Evaluated?
This is one of the most overlooked causes of IVF failure.
Doctors reassess:
- Sperm DNA fragmentation
- Lifestyle damage (smoking, heat exposure, stress)
- Whether IVF was sufficient or ICSI was medically required
Important truth:
A “normal semen analysis” does not guarantee healthy sperm DNA.
Poor DNA quality is a common reason for repeated IVF failure.
5. Should the Same Stimulation Protocol Be Repeated?
Repeating the same injections without review is a warning sign.
Doctors evaluate:
- Egg quality, not just egg count
- Whether over-stimulation harmed egg health
- If a milder stimulation approach would be more effective
Straight fact:
More injections do not automatically mean better results.
6. Was Embryo Transfer Timing Accurate?
Implantation occurs within a very narrow window.
Doctors review:
- Whether the transfer day was chosen correctly
- Synchronization between embryo age and uterine readiness
- If frozen embryo transfer would allow better timing control
Clinical reality:
A timing mismatch of even 12–24 hours can cause IVF failure.
7. Immune or Blood-Clotting Factors (Only When Indicated)
Not every patient needs advanced testing.
Doctors consider these only if:
- There is repeated implantation failure
- Autoimmune disease is suspected
- There is a clinical reason to test for clotting disorders
Warning:
Empirical immune treatment without diagnosis is poor medical practice.
8. Physical and Mental Burnout Is a Medical Factor
This is not emotional counselling—it is clinical reality.
Doctors observe:
- Sleep disturbances and weight changes
- Poor response to hormones
- Difficulty following treatment protocols
Truth:
Sometimes taking a short medical pause improves the next cycle outcome.
9. When Strategy Must Change, Not Just the Cycle
After IVF failure, experienced doctors may:
- Switch to frozen embryo transfer
- Correct male factor aggressively
- Recommend genetic testing only when clearly indicated
Key rule:
If nothing changes, results will not change.
Common Myths Patients Must Stop Believing
- “My body rejected the embryo” – incorrect
- “One failure means IVF will never work for me” – false
- “More cycles automatically increase success” – dangerous thinking
IVF is a medical process, not a gamble.
Final Message
IVF failure is not the end—but repeating cycles blindly is a medical mistake.
Good IVF doctors:
- Do not promise guarantees
- Identify what went wrong
- Correct problems before the next attempt
If your IVF has failed once or twice, the answer is not “try again quickly.”
The correct step is to understand what was missed—and fix it properly.
FAQs
1. What should be done if IVF failed once or twice?
If IVF failed once or twice, the next step should not be an immediate repeat cycle. Doctors first review hormones, embryo quality, uterine readiness, transfer timing, and male factors to identify what went wrong before planning the next attempt.
2. Is it normal for IVF to fail in the first or second attempt?
Yes. IVF failure in the first or second attempt is medically common. Success depends on multiple factors such as egg quality, sperm DNA, lab conditions, and implantation timing. One or two failures do not mean IVF will never work.
3. Can good-quality embryos still fail to implant?
Yes. Even good-quality embryos can fail if the uterine lining is not receptive, progesterone timing is incorrect, or embryo–uterus synchronization is off. Implantation depends on more than embryo appearance alone.
4. Should the same IVF protocol be repeated after a failed cycle?
Not always. Repeating the same protocol without review is a medical risk. Doctors usually reassess stimulation drugs, doses, egg quality, and response before deciding whether the protocol should be changed.
5. Does male factor matter after IVF failure?
Yes. Male factors are often overlooked after the first failure. Sperm DNA fragmentation and lifestyle-related damage can cause repeated IVF failure even when standard semen analysis looks normal.
6. How long should one wait before starting the next IVF cycle after failure?
There is no fixed rule. Some patients can proceed in the next cycle, while others benefit from a short medical pause to correct hormonal imbalance, improve health, or change strategy. The decision should be individualized.